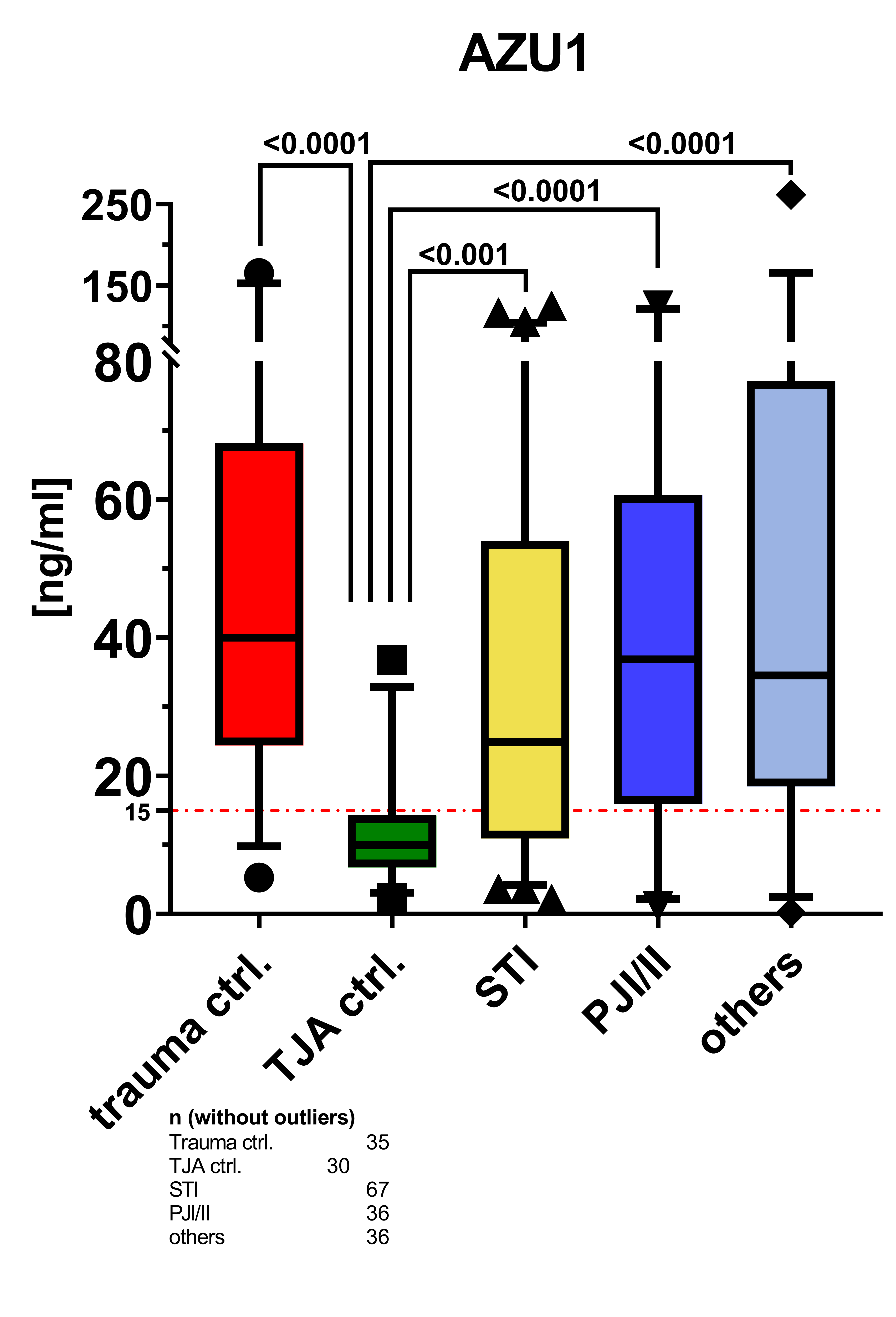
AZU1: a new promising marker for infection in orthopedic and trauma patients?
DOI:
https://doi.org/10.17179/excli2023-6705Keywords:
AZU1, HBP, orthopedic surgery, infection, trauma surgeryAbstract
Early and reliable detection of infection is vital for successful treatment. Serum markers such as C-reactive protein (CRP) and procalcitonin (PCT) are known to increase with a time lag. Azurocidin 1 (AZU1) has emerged as a promising marker for septic patients, but its diagnostic value in orthopedic and trauma patients remains unexplored. Between July 2020 and August 2023, all patients necessitating inpatient treatment for periprosthetic joint infection (PJI), peri-implant infection (II), soft tissue infection, chronic osteomyelitis, septic arthrodesis, bone non-union with and without infection were enrolled. Patients undergoing elective total joint arthroplasty (TJA) served as the control group. Blood samples were collected and analyzed for CRP, white blood cell count (WBC), PCT, and AZU1. Based on the inclusion and exclusion criteria 222 patients were included in the study (trauma = 38, soft tissue infection = 75, TJA = 33, PJI/II = 39, others = 37). While sensitivity and specificity were comparably high for AZU1 (0.734/0.833), CRP and PCT had higher specificity (0.542/1 and 0.431/1, respectively), and WBC a slightly higher sensitivity (0.814/0.455) for septic conditions. Taken together, the area under the curve (AUC) showed the highest accuracy for AZU1 (0.790), followed by CRP (0.776), WBC (0.641), and PCT (0.656). The Youden-Index was 0.57 for AZU1, 0.54 for CRP, 0.27 for WBC, and 0.43 for PCT. Elevated AZU1 levels effectively distinguished patients with a healthy condition from those suffering from infection. However, there is evidence suggesting that trauma may influence the release of AZU1. Additional research is needed to validate the diagnostic value of this new biomarker and further explore its potential clinical applications.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Philipp Hemmann, Lisa Kloppenburg, Regina Breinbauer, Sabrina Ehnert, Gunnar Blumenstock, Marie K. Reumann, Felix Erne, Johann Jazewitsch, Tobias Schwarz, Heiko Baumgartner, Tina Histing, Mika Rollmann, Andreas K. Nüssler

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish in this journal agree to the following terms:
- The authors keep the copyright and grant the journal the right of first publication under the terms of the Creative Commons Attribution license, CC BY 4.0. This licencse permits unrestricted use, distribution and reproduction in any medium, provided that the original work is properly cited.
- The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations.
- Because the advice and information in this journal are believed to be true and accurate at the time of publication, neither the authors, the editors, nor the publisher accept any legal responsibility for any errors or omissions presented in the publication. The publisher makes no guarantee, express or implied, with respect to the material contained herein.
- The authors can enter into additional contracts for the non-exclusive distribution of the journal's published version by citing the initial publication in this journal (e.g. publishing in an institutional repository or in a book).