Case report
Pseudomonas aeruginosa bacteremia secondary to acute right leg cellulitis: case of community-acquired infection
Asrul Abdul Wahab1[*], M.M. Rahman1
1Department of Medical Microbiology and Immunology, Faculty of Medicine, The National University of Malaysia, Cheras 56000 Kuala Lumpur, MalaysiaEXCLI J 2013;12:Doc997
Abstract
Pseudomonas aeruginosa is a gram-negative bacillus that causes wide spectrum clinical infections. However, it is most frequently associated with hospital-acquired infection. In this case a 58-year-old male with underlying hypertension and dyslipidaemia was admitted for acute right leg cellulitis. Pseudomonas aeruginosa was identified from the case, though it was not a usual suspected organism. It might be due to community-acquired infection.
Keywords: AmpC, bacteremia, cellulitis, community-acquired, Pseudomonas aeruginosa
Introduction
Pseudomonas aeruginosa is a gram-negative bacillus that commonly colonizes hospital environment. It contaminates water and hospital devices and is known as aetiological agent of nosocomial infection. Community-acquired infection of this organism had been reported (Hadi et al., 2007[5]). The prevalence of P. aeruginosa bacteremia varies from one to other institutions and the sources of bacteremia were identified in 66 % of cases (Vitkauskiene et al., 2010[11]). Altogether 21% of these bacterial infections were classified as community-acquired infection (Parkins et al., 2010[7]).
Case Report
A 58-year-old Malay male with background medical problem of hypertension and dyslipidemia presented with fever and right leg swelling for three days duration prior to admission. The fever was described as a high grade and it was associated with chills and rigors. It started together with the right leg swelling. The right leg swelling was sudden onset and it was associated with severe throbbing pain. There was no prior history of trauma and insect bite. This was his first episode of leg swelling. There was neither chest pain nor shortness of breath. Because of that he had some difficulty while walking. On clinical examination, he was alert and conscious but febrile with body temperature of 38 °C. His blood pressure was normal but he was tachycardic with heart rate of 130 beats per minute. His respiratory rate was normal. Respiratory and cardiovascular system examination revealed no abnormality. Right leg examination revealed swelling of the right leg with erythematous skin. There was no blister. There was no clear demarcation with the surrounding skin. The right leg was not gangrenous and no trauma or bite mark was seen. It was tender on palpation but there was no crepitus. The peripheral pulses were present. Ultrasound Doppler of the right leg showed no evidence of deep vein thrombosis and no osteomyelitis changes of the right tibia and fibula were noted by x-ray. His total white cell count was within normal limit but the neutrophil level was elevated. The hemoglobin and platelet level were normal. C-reactive protein was markedly elevated at 23.8 mg/dL. His random blood sugar was within normal range. ECG showed sinus tachycardia with no other abnormality. The diagnosis of acute right leg cellulitis was made. Empirical antibiotics consisting of intravenous c-penicillin and cloxacillins were applied.
Blood sample from the patient was sent for culture on the day of admission, grew gram-negative rods after one day of incubation. These were then identified as Pseudomonas aeruginosa based on the typical morphological features. The organism produced hemolytic colonies on blood agar and greenish diffusible pigment seen on the Muller Hinton Agar (MHA) with typical odor of Pseudomonas aeruginosa. It was non-lactose fermenter with alkaline reactions at both butt and slant in the triple sugar iron agar. The organism was motile and the cytochrome oxidase was positive. The organism was an AmpC producer. The patient was not responding to the empirical antibiotics and they were judiciously replaced by intravenous cefepime 1 gram 12 hourly. Subsequently, his condition improved and the right leg cellulitis was gradually resolved. The C-reactive protein and white cell counts also were decreasing in trend as shown in Table 1(Tab. 1). Intravenous cefepime was continued for 14 days. Repeated blood cultures on day five of treatment and before discharge were negative. He was discharged well.
Discussion
Pseudomonas aeruginosa is a leading cause of nosocomial infection and associated with high mortality rate (Fazlul et al., 2011[3]). Pneumonia and sepsis are the most common infections associated with these bacteria (Tam et al., 2009[9]). This is a case of Pseudomonas aeruginosa bacteremia, which we believe might have acquired from community setting. Pseudomonas aeruginosa is an uncommon cause of community-acquired bacteremia. Cases of community-acquired P. aeruginosa bacteremia represent about 21 % of all cases of P. aeruginosa bacteremia (Parkins et al., 2010[7]). Community-acquired P. aeruginosa infections occurred in those with specific predisposing factors such as neutropenic and chronic structural lung diseases such as cystic fibrosis and bronchitis (Schechner et al., 2009[8]). In our case, we could not find any significant risk factors that are associated with community-acquired P. aeruginosa infection.
From hospital-based study, P. aeruginosa accounted around 2.7 % of all bacteremia cases and the primary source is identified in 60 to 70 % of the cases, with respiratory tract as most common site of infection (Vitkauskiene et al., 2010[11]). Most of the time, community-acquired P. aeruginosa infection presents as otitis externa (Hadi et al., 2007[5]). Staphylococcus aureus and beta hemolytic streptococci are the most common aetiological agents for cellulitis and P. aeruginosa is not a common cause of cellulitis (Dryden et al., 2009[2]). P. aeruginosa was not suspected in our case at the time of presentation due to this knowledge. Skin and soft tissue infections caused by this organism can appear as primary or metastatic foci, expressed in wide presentations including cellulitis, ecthyma gangrenosum, necrotizing fascitis and gangrene (Giamerellou, 2000[4]). Independent predictors of P. aeruginosa bacteremia in community setting were severe immunodeficiency, age >90 years, receipt of antimicrobial therapy within past 30 days, and presence of central venous catheter or urinary device (Schechner et al., 2009[8]). None of these factors was identified for our patient. Perhaps, molecular methods are the most appropriate investigational tool to identify clusters of Pseudomonas aeruginosa that belong to community or hospital-acquired skin and soft tissue infection in origin (Hadi et al., 2007[5]).
Treatment of P. aeruginosa is always challenging because these bacteria can easily develop resistance to many classes of antibiotics. P. aeruginosa is known to possess many resistance genes thus it is associated with multiple mechanisms of antibiotic resistance (Tam et al., 2007[10]). Over-expression of AmpC is one of the resistance mechanisms that commonly exist in P. aeruginosa. We were able to see the similar phenotype of AmpC overexpression in our isolate in this case. The patient responded well to the treatment and completed the antibiotic course for 14 days. Repeated blood culture showed a negative result indicating a successful treatment. AmpC overexpression was found to be associated with non-susceptibility to ciprofloxacin by Cabot et al., 2011[1]. However this association did not occur in this case as the organism is still susceptible to ciprofloxacin.
The prognosis of P. aeruginosa bacteremia varies from one hospital to another. The 30-day mortality rate shown by a study in Japan was 20.9 % with thrombocytopenia and polymicrobial infections as the significantly contributing factors (Horino et al., 2012[6]). Perhaps, absence of these two factors could contribute to better outcome in our case.
Conclusion
Pseudomonas aeruginosa is not a common aetiological agent of community-acquired skin and soft tissue infection with bacteremia. Its infections in community should be managed cautiously particularly in high-risk populations those are immunosuppressant. Treatment of Pseudomonas aeruginosa infection is always challenging as the organism easily acquires resistance to different classes of antibiotics.
Acknowledgement
Authors thank the Dean of the Faculty of Medicine and the Head of the Department of Medical Microbiology and Immunology, The National University of Malaysia for cooperation and help.
References
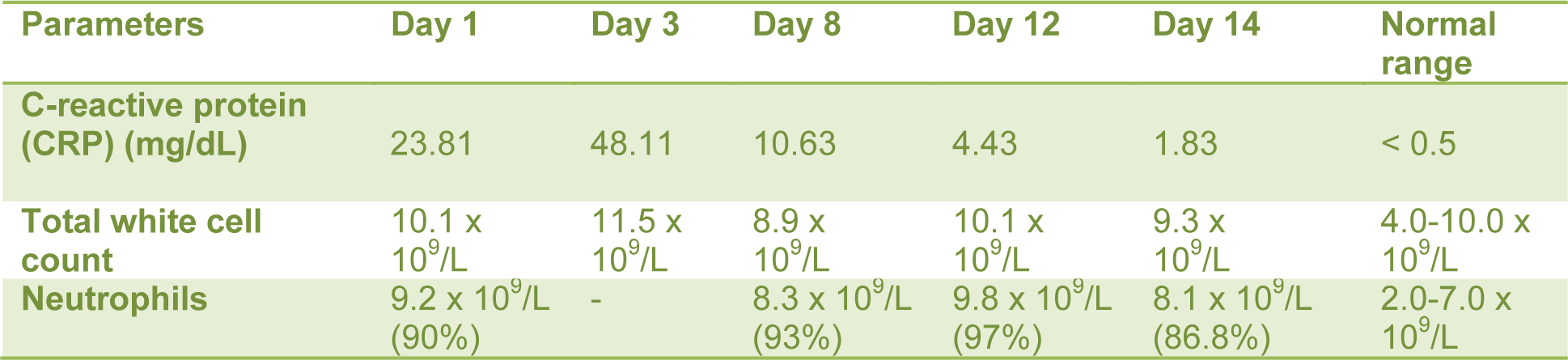
Table 1: C-reactive protein (CRP), total white cell count and neutrophils count from day of admission (Day 1) until Day 14
[*] Corresponding Author:
Asrul Abdul Wahab, Department of Medical Microbiology and Immunology, Faculty of Medicine, The National University of Malaysia, Cheras 56000 Kuala Lumpur, Malaysia; Tel: +603-91455927, eMail: asrulwahab@hotmail.com